Provider Directory Software | symplr Directory
Centralize provider data to power mission-critical systems
Harness the power of accurate, integrated data
... and give patients the modern-day consumer experience they expect!
- Enable online appointment booking
- Reduce call center volume
- Drive accurate patient-provider matching
Plus, quickly add referring providers to your EHR and avoid reimbursement delays.

Give your provider, patients, and payers a better experience using precise provider data
Health systems rely on electronic health records (EHRs) to manage patient data, yet lack a single source of truth for provider data. Instead, departments across health systems manage provider data in silos. The results:
- Inaccurate provider data in critical systems
- Delayed and lost revenue
- Patient leakage
- Disgruntled providers
What healthcare leaders often don't realize is that by centralizing provider data, they can make a meaningful impact on mission-critical challenges. Simply put, deploying a single system for managing provider data makes healthcare operations more effective.
symplr Directory consolidates provider data into a single, centralized solution. With its easy-to-use interface, maintaining profiles for every credentialed and referring provider across the enterprise is simple. By implementing symplr Directory, you can quickly reduce inaccurate provider data, eliminate record duplication, and securely share provider information with all departments and software solutions that rely on it, including your EHR.
That means your providers spend less time on administrative work, and staff spend less time adding referring provider information into the EHR. Reimbursement is quicker, call center volume decreases, you accommodate more new patients, and patient leakage decreases.

RECOGNIZED AND VERIFIED WITH INDUSTRY AWARDS
Achievement in Product Innovation
Stevie Award
Best Provider Data Management Platform
MedTech Breakthrough Award
Accelerate digital transformation using high-quality provider data
Integrate and maintain accurate provider data in a central hub
Grow net patient revenue by keeping patients in-network
Optimize your digital front door to deliver a better customer experience
Unlock the potential of your provider data
National Provider Network
Reduce billing delays by enrolling referring providers in real time by performing a quick search of the symplr Directory National Provider Network. Find referring providers and add their profile to your EHR with a click of a button.
Schedule Advisor
Provider Outreach
WebMD's Care Finder Direct Integration
Robust Reporting
Clinical Taxonomy
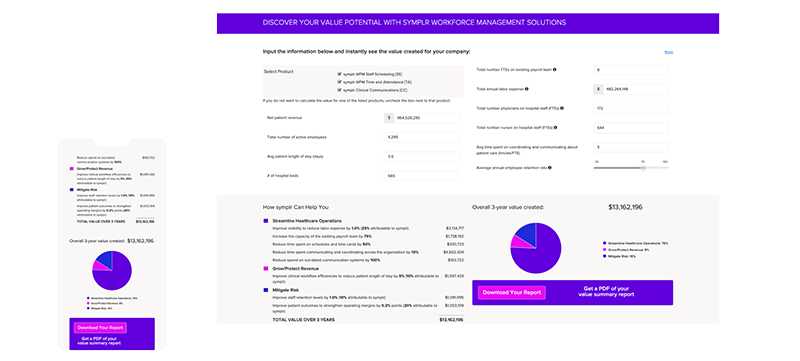
Calculate the value symplr Directory would add to your health system
Enter a few data points into our calculator to estimate cost savings and additional revenue your health system can generate with symplr Directory.
What our symplr Directory customers are saying
Break down data silos to boost operational efficiency
“We now have high-quality provider data due to multiple teams curating data in symplr Directory. Data is being fed continuously to symplr Directory from trusted sources.”